Source: www.healio.com
Author: Matthew Shinkle
Key takeaways:
- Researchers saw no statistical difference between patient groups with respect to treatment outcomes.
- Larger studies are needed to further evaluate this study’s findings.
Compared with expectant management, imaging-based surveillance did not improve outcomes among patients in remission after completion of primary radiation therapy for head and neck cancer, according to data published in JAMA Network Open.
Although imaging “in the context of clinical suspicion” for this specific patient population is common and typically beneficial, according to researchers, the results of this study show that such a practice is not valuable for asymptomatic patients.
“The results of the present study, while seemingly paradoxical, are consistent with those of others which have failed to demonstrate a benefit to surveillance imaging among patients who have successfully completed treatment for head and neck cancer,” Allen M. Chen, MD, MBA, professor and chair of the department of radiation oncology at University of California, Irvine, Chao Family Comprehensive Cancer Center, and researchers wrote.
Researchers conducted a retrospective, comparative effectiveness review to evaluate the potential benefit of surveillance imaging among asymptomatic patients with head and neck cancer currently in remission following completion of chemoradiation.
The study included 340 adults (59% men; 43% white) who had achieved a complete metabolic response to initial treatment for newly diagnosed squamous cell carcinoma of the head and neck between January 2014 and June 2022.
Researchers defined surveillance imaging as the acquisition of a PET with CT, MRI or CT of the head and neck region in the absence of clinically suspicious symptoms and/or examination findings.
Local-regional control, OS and PFS based on assignment to either the surveillance imaging or expectant management cohort served as the study’s main outcome measurements.
Of the 340 patients, 187 underwent imaging-based surveillance (55%) and 153 (45%) received expectant management.
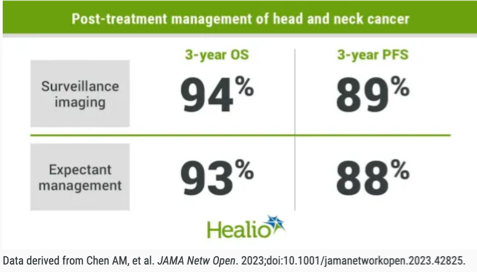
Researchers observed no statistically significant difference in outcomes between the surveillance imaging or expectant management cohorts in 3-year local-regional control (90% vs. 93%), OS (94% vs. 93%), PFS (89% vs. 88%) or freedom from distant metastasis (90% vs. 90%).
Researchers noted a few study limitations, including being a nonrandomized trial that selected patients with “relatively favorable prognosis from the onset,” they wrote. Additionally, potential evidence of treatment-related sequelae could have caused some patients to be symptomatic and no policy had been in place to direct acquisition of additional imaging following the initial PET/CT.
Additional research will still be needed to understand the full implications and impact of not undergoing routine imaging-based surveillance, but researchers say the results still provide compelling evidence that patients in the surveillance imaging cohort saw no benefit.
“While a discussion regarding the implications with respect to cost-effectiveness lies beyond the scope of this work and has been reported by others, most patients in this study underwent routine surveillance for no apparent benefit,” Chen and researchers wrote. “Additional studies that take into account the probability of recurrence, the distribution of metastatic disease, and the availability of effective therapies for recurrent disease are needed to gauge its true effectiveness. Larger, multi-institutional studies are needed to further evaluate our findings.”
Source:
Chen AM, et al. JAMA Netw Open. 2023;doi:10.1001/jamanetworkopen.2023.42825.
Disclosures: All authors report no relevant financial disclosures.

Leave A Comment
You must be logged in to post a comment.