Henderson throat cancer patient rallies after cutting-edge treatment
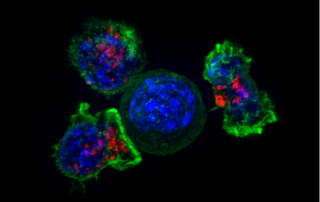
Source: www.reviewjournal.com Author: Mary Hynes, Las Vegas Review-Journal In February, a cancerous tumor caused extreme swelling in Ruben Solis’ neck and face, blocking his airway. After an emergency tracheotomy, an incision to his windpipe that allowed him to breathe, Solis had to decide whether he wanted to enter a clinical trial to receive an experimental treatment. The 54-year-old Henderson resident was skeptical. But with stage 4 laryngeal cancer that had spread to his lungs, he was running out of options. Three months later, after three treatments, the tumors in his throat and lungs have dramatically shrunk and the swelling subsided. “I feel much better,” Solis said Monday. The father and grandfather, who worked in banquets and as a food and beverage manager on the Strip before falling ill, is the first person in the world to receive a combination of two experimental drugs, Enoblituzumab and Retifanlimab, as part of a new clinical trial for head and neck cancer, according to Comprehensive Cancer Centers of Nevada, the local site participating in the global study. Solis and his oncologist, Dr. Anthony Nguyen, spoke with reporters prior to the patient receiving his fourth infusion of the two drugs. The treatment is a new form of immunotherapy, which boosts the body’s immune system to combat the cancer. “So his immune system is actually being manipulated, turned on, to actually fight the cancer from inside,” Nguyen said. In this way it is different from traditional chemotherapy. “When we think of chemotherapy and cancer medicine, we [...]