Genetic changes in head and neck cancer, immunotherapy resistance identified
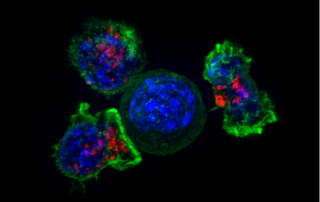
Source: MedicalXPress Date: April 26th, 2021 Author: University of San Diego-California A multi-institutional team of researchers has identified both the genetic abnormalities that drive pre-cancer cells into becoming an invasive type of head and neck cancer and patients who are least likely to respond to immunotherapy. "Through a series of surprises, we followed clues that focused more and more tightly on specific genetic imbalances and their role in the effects of specific immune components in tumor development," said co-principal investigator Webster Cavenee, Ph.D., Distinguished Professor Emeritus at University of California San Diego School of Medicine. "The genetic abnormalities we identified drive changes in the immune cell composition of the tumors that, in turn, dictates responsiveness to standard of care immune checkpoint inhibitors." Reporting in the April 26, 2021 online issue of the Proceedings of the National Academy of Sciences, researchers describe the role of somatic copy-number alterations—abnormalities that result in the loss or gain in a copy of a gene—and the loss of chromosome 9p in the development of human papillomavirus (HPV)-negative head and neck cancer. The loss of chromosome 9p and the deletion of JAK2 and PD-LI, two neighboring genes found on chromosome 9p, was associated with resistance to immune checkpoint inhibitors, a type of cancer immunotherapy that uses antibodies to make tumor cells visible to a patient's immune system. "Although programmed death-1 (PD-1) immune checkpoint inhibitors represent a major breakthrough in cancer treatment, only 15 percent of patients with HPV-negative head and neck cancer respond to treatment," said [...]