Susan Smith noticed a small bump on the side of her tongue that hurt when she ate. When she visited her dentist for a check-up, she mentioned it. The dentist wasn’t too worried but recommended Smith see an ear, nose and throat doctor. Over the next five months, she saw three doctors who had her try various mouth rinses. Still, the lump remained.
Finally, a fourth doctor sent her for a CT scan, and Smith learned what was wrong: She had tongue cancer.
“What was on the surface of my tongue was the tip of the iceberg, and I actually had a four-centimeter mass that was inside the tongue into the floor of my mouth,” Smith, 48, of Fairfield, Connecticut, tells TODAY.com. “They diagnosed me as having stage 4A tongue cancer that spread to the lymph nodes in my neck.”

Smith is part of a group called Young Tongues. They’ve noticed that tongue cancer, which has historically impacted older men who drink and smoke, seems to be occurring in younger patients. Emerging data reveals that the demographic of tongue cancer patients is changing, but experts are unsure why. For patients, that can mean months of being misdiagnosed or ignored before ultimately receiving the proper diagnosis.
“I felt dismissed,” Smith says. “Anger followed pretty quickly after that because I was so far along. I was stage 4A.”
Bump on the tongue, ear pain
The bump on Smith’s tongue mostly hurt when she ate. She also experienced almost constant ear pain.
“I started to get a really strange earache that wouldn’t go away,” she says.
After mentioning it to her dentist, Smith scheduled a visit with an ear, nose and throat doctor.
“I saw not one but three, and every single one I went to said that they just thought it was an irritation on my tongue and to try rinses or that they were sure it would go away,” Smith explains. “It kept getting bigger, and it kept hurting more.”
It felt frustrating that the doctors offered few answers.
“I didn’t feel like the doctor was listening,” Smith says. “It was a struggle to get doctors to pay attention.”
The third doctor she saw performed a biopsy that came back as benign. Then the COVID-19 pandemic started, pausing her search for a diangosis. When she could resume doctor’s visits, she saw a fourth who sent her for a CT scan.
“He took one look at me and said, ‘We have a problem,’” she says. “I felt elated that someone was finally listening to me and slightly vindicated because I felt in my heart of hearts something was wrong. I was losing weight at that point, like rapidly, for no reason.”
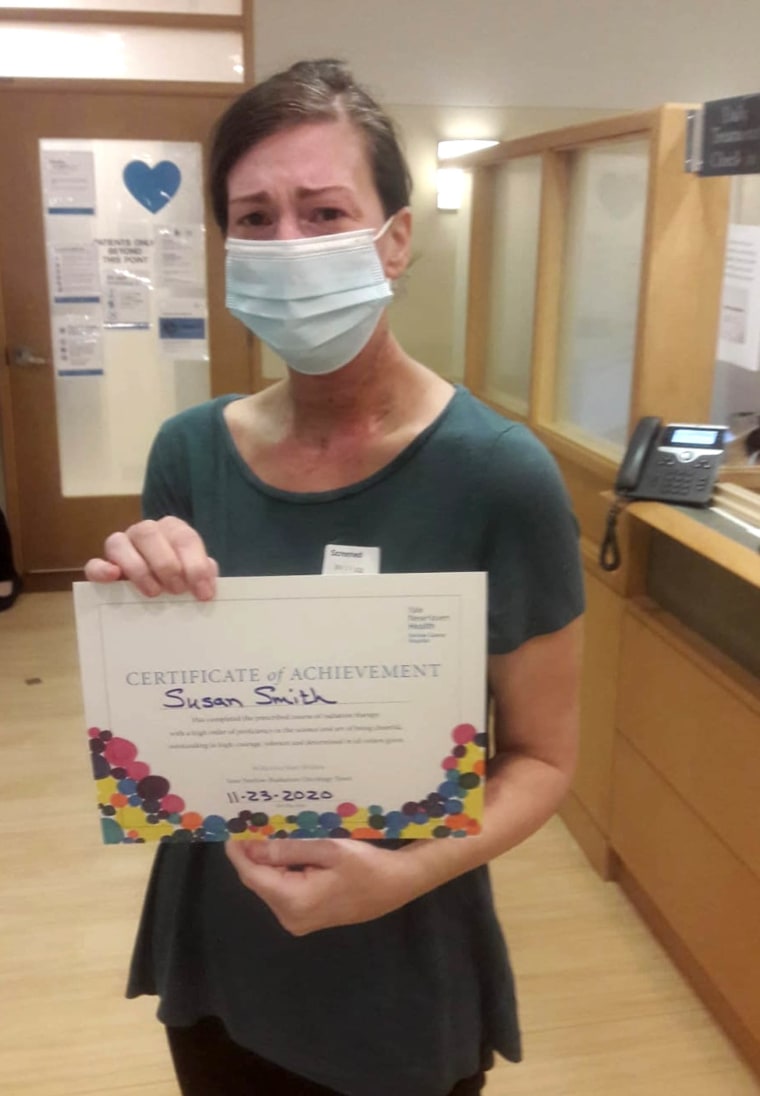
To treat her cancer, Smith underwent a 15-hour surgery where doctors removed a third of her tongue and reconstructed it with a skin graft on her left arm. She also had to have a neck dissection — “where they actually cut from your ear all the way to the front of your neck,” to remove 36 lymph nodes. After six weeks of recovery, she started six weeks of radiation and chemotherapy concurrently.
Treatment felt tough. “You very much lose the ability to speak coherently,” Smith recalls. “It takes a long time to build back up to be able to speak normally, or as close to normal as possible.”
Radiation burned the inside of her mouth and throat, making eating painful. She also lost her sense of taste. She lost 52 pounds.
“Most things (tasted) like cardboard,” she says. “It hurts so bad to eat and swallowing becomes so difficult because of the inflammation happening in your mouth and throat and then added to that is the psychological impact of not tasting your food.”
Eventually, Smith was hospitalized for malnutrition.
“I had stopped eating for 11 days,” she says.
Smith felt surprised she was diagnosed with tongue cancer because she did not match the profile of the typical patient. Soon after, she discovered the Young Tongues, which includes young people with tongue cancer worldwide. One of its founders, Barbara Fountain, says the group has experienced an influx of members. But the reason tongue cancer is impacting younger people seems unclear.
“There is a mystery as to why more and more young people — and actually statistically more female, younger people — are getting diagnosed with tongue cancer,” Fountain, 26, of Norwich, England, tells TODAY.com. “(In younger populations) you’re not really able to smoke enough, to drink enough to cause that type of damage.”
Fountain received any early diagnosis after an ulcer on her tongue wouldn’t go away. After only three months, the then 22-year-old learned she had stage 1 tongue cancer.
“I seem to be even more of a rarity because my cancer got caught early, which makes a really big impact in terms of outcomes from survival rates and quality of life,” Fountain says. “A lot of young women don’t get referred to a specialist quick enough. … I was just plain lucky that my dentist follows best practices.”
An increase in tongue cancer in young patients
For years, Dr. Diana Kirke noticed a difference in some of her tongue cancer patients. They were in their 20s, 30s and 40s and didn’t use tobacco or imbibe heavily.
Typical tongue cancer patients “are older males who smoke and drink and occasionally elderly females with probably a dental issue and therefore a predilection to developing a tongue cancer,” Kirke, an otolaryngologist at Mount Sinai Hospital, tells TODAY.com.
“Since 2010, there seems to be a national shift to younger patients developing oral tongue squamous cell carcinoma. There is a very clear rise in patients that are non-smokers and non-drinkers.”
Until recently, though, there wasn’t much data to support what she was seeing. A few weeks ago, Kirke and her colleagues presented an abstract at an American Head and Neck Society conference that showed regional areas with higher numbers of young people with tongue cancer, what they call hotspots.
“(One of our papers) was trying to understand whether there are environmental hotspots for the development of oral cancer in young patients,” she says.

Their paper looked at data from 2000 to 2019 on patients aged 14 to 44 from 17 cancer registries from 13 states. Not every state or city catalogues cancer the same way, which limits the information Kirke can gather. While they did find some hotspots, the picture remains incomplete.
“For instance, Los Angeles was a hotspot, but it’s probably because they have an excellent university health system,” she explains. “New Haven was a hotspot, but that’s probably because of Yale.”
They hope to find more robust data from other locations to include in their research. Still, experts can’t point to a reason behind this shift in tongue cancer patients.
“We really don’t have a good, causative reason as to why,” Kirke says.
She says another paper from researchers from the University of Kansas looked at issues diagnosing young people with tongue cancer. It found what Smith experienced — there’s a delay in diagnosis.
“It takes a long time for their tumor to be diagnosed, and I suspect because it’s not being considered,” Kirke says. The study also found that “time from onset to biopsy was 30 weeks.”
Researchers are looking for reasons why tongue cancer is impacting a different patient population. Dr. Richard Bakst is examining the oral microbiome to see if something in it might contribute a person developing tongue cancer.
“Everyone who comes into my office asks, ‘How did I get this?’ And the answer to 98% of those questions is, ‘I don’t know,’” Bakst, a radiation oncologist from Mount Sinai Hospital, tells TODAY.com. “The next question is, ‘What could I do about my risk?’ And there’s really not much that we have to offer.”
So, he began considering whether something in the oral microbiome might be contributing to this trend. He and his colleagues are currently recruiting healthy patients and those with tongue cancer within Mount Sinai to obtain samples of their microbiome to analyze. They hope that having a more complete understanding of the oral microbiome can help doctors understand why some young people are developing tongue cancer — or find different treatments.
“The first question we’re asking is: What are the ‘bad species’ of microorganisms? And the second question we’re going to ask: Is why are they bad? What are they doing?” he says. “It may go beyond, ‘You have this bacteria so you’re at risk.’”
Advocacy and support
While getting an early diagnosis made a difference in Fountain’s outcome, her experience with tongue cancer still felt tough.

“It was a very lonely, isolated experience,” she says. “My waiting room was full of 80-something-year-olds.”

That contributed, in part, to her starting Young Tongues. The group helps people grapple with a cancer more often found in older people and survivorship. Some people lose their taste for the rest of their lives or experience lifelong dental and mouth problems.
“You’re not just looking at getting through the treatment and surviving. You’re also looking at the quality of life after,” Fountain says, such as tooth loss, changes to the jaw bones and gum recession.
It’s been two years since Smith underwent treatment for her tongue cancer. She’s cancer free and will undergo heightened surveillance for another three years. Having support from others, including the Young Tongues, helped her tremendously.
“Every cancer has such an impact. But for head and neck cancer, your mouth is how you communicate. It’s how you eat and nourish yourself,” she says. “It’s a different kind of cancer because it has such an impact on your daily life and how you socialize (and connect) with people. To have a group of people who understand that impact was really monumental.”

Leave A Comment
You must be logged in to post a comment.