Source: www.nationalgeographic.co.uk
Author: Sanjay Mishra
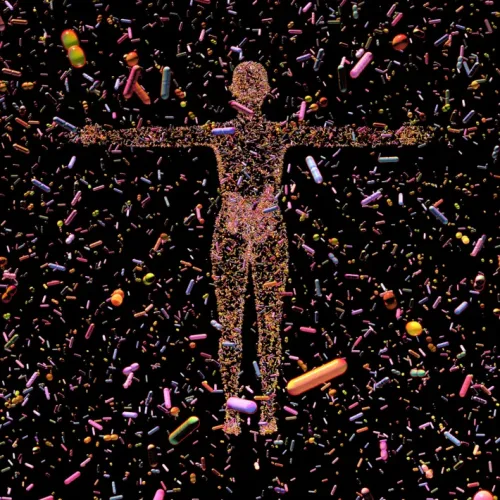
An unfathonable number of bacteria, live in and on our bodies; most providing some benefits. Now researchers have discovered that some species of bacteria are actually protecting cancer cells. This finding could inspire new strategies to fight cancer.
Photograph by illustration by Russell Kightley, Science Photo Library
Most bacteria living in the human body help us thrive, but recent studies show that some infiltrate tumours, helping them grow, spread, and become more difficult for the immune system to destroy.
The human body contains 100 trillion or so microbial cells, almost as many, if not more, than the number of human cells in the body. Bacteria make up most of this microbiome, living in our gut, on our skin, in the respiratory and urogenital tracts, and in mammary glands. A number of recent studies have revealed that bacteria are also present in a wide variety of tumours, where they live not only between cells but even inside them. The bacteria were thought to be taking advantage of a favourable growing environment; scientists had no idea whether these microbes could alter cancer prognosis.
Now a study published recently in Nature shows that bacteria in oral and colorectal tumors can directly promote cancer by suppressing the human immune response and helping cancer cells spread more rapidly. An accompanying study published in the journal Cell Reports finds that some anticancer drugs, such as 5-fluorouracil, may be effective because they also kill the bacteria which help the tumour develop.
“Our data suggests that bacteria are not innocent bystanders but instead are shaping the ecosystem in the regions of the tumour where they were located,” says Susan Bullman, a microbiologist at the Fred Hutchinson Cancer Centre in Seattle, who led both studies. “Bacteria are a viable part of this tumor microenvironment.”
Jennifer Wargo, a surgical oncologist at the University of Texas MD Anderson Cancer Centre in Houston, says that there was a lot of skepticism of previous studies showing there might be bacteria and other microbes in the tumours. In 2017, she discovered that if patients with melanoma have a more diverse population, or an abundance, of “good” bacteria in their guts, they respond better to immunotherapy.
“We even find microbes within brain tumours. You’re like, gosh, how did they get there?”
The new study of oral and colorectal tumours “pretty conclusively shows that not only there are microbes within tumours, but they can actually be within cancer cells themselves, and even within immune cells,” says Wargo, who leads the Platform for Innovative Microbiome and Translational Research at MD Anderson.
This study shows that bacteria and tumours co-exist and cooperate to promote cancer progression with the location of bacteria being an important factor, says Toni Choueiri, an oncologist at Dana-Farber Cancer Institute in Boston who has led trials of many now-approved genitourinary and kidney cancer treatments. He adds that Bullman’s studies should help to convince scientists that the presence of bacteria in tumours might not be random at all.
Together these two studies suggest that understanding the relationship between tumours and their resident microbes could be vital for fighting and eliminating certain cancers.
Bacteria can boost or block cancer growth
That bacteria can somehow affect the course of cancers has been suspected since late 19th century when German physicians Wilhelm Busch and Friedrich Fehleisen independently found that patients’ tumors sometimes shrank after they had a bout of erysipelas, a skin condition triggered by Streptococci bacteria. Following dozens of such observations, William Coley developed his cocktail of heat-killed bacteria, called “Coley’s Toxins,” to treat patients with osteosarcoma, but with limited success. This cocktail has since been abandoned because it carried the risks of fatal infection.
Unlike the Streptococcus species causing erysipelas, which helped to fight tumours, the bacterium Helicobacter pylori is classified as a carcinogen because some scientists think it causes gastric tumors, although this is hotly debated.
An oral bacterium called Fusobacterium nucleatum is frequently found in many gastrointestinal tract tumors where its presence is associated with poor prognosis and treatment failure. Studies have also suggested that dysbiosis—an imbalance of the gut microbial community—can drive gastrointestinal cancers. Conversely, the presence of certain bacteria in a patient’s gut boosts the success of immunotherapy.
Following these leads, Bullman found in a 2017 study published in Science that Fusobacterium nucleatum and other bacteria were not only present in the primary colorectal tumors but also in metastatic cancer cells that spread far from the original tumour.
When Bullman implanted a patient’s tumour containing Fusobacterium into mice and gave them antibiotics, it not only killed the bacteria but also decreased the tumour size, highlighting that Fusobacterium was somehow associated with the growth and survival of the cancer.
“Over 10 years ago, advances and accessibility in sequencing technologies had hinted at the possibility of bacterial communities residing within human tumor tissue,” Bullman says, “but there was very little known about how these microbes got there and what they were doing. We didn’t have the tools or technologies that allowed us to look at this component of the tumour.”
Drugs that kill microbes and tumours
If bacteria contributed to cancer initiation or progression, Bullman thought, targeting the microbes could help treat and possibly prevent cancers. But nobody knew how the bacteria might shape the microenvironment of the tumour cell.
To figure it out, Bullman teamed up with Christopher Johnston, also a molecular microbiologist from Fred Hutch. They focused on two types of oral and colorectal cancer tumours since bacteria were already implicated in their development.
Bullman and Johnston’s team collected tumour samples from 11 patients and split each sample into four pieces of tissue. They used a standard method called 16S ribosomal DNA (rDNA) analysis to identify and characterise all the bacteria in the tumour samples; Fusobacterium was the most prevalent bacterium.
But when scientists probed the slices of tumour tissue with higher resolution methods, they discovered that bacteria were not distributed uniformly through the tumours. In fact, most patients had very uneven distribution of bacteria in tumour tissue.
“We saw bacterial hotspots,” Johnston says.
They found that areas of tumours that contained bacteria were generally more immunosuppressed than the bacteria-free areas. Parts of tumour with more bacteria had fewer blood vessels; lower levels of immune cells called T cells, which destroy cancer; and higher levels of myeloid cells, which promote tumour growth by suppressing immunity. Cancer cells in bacteria-rich regions also had a greater capacity to proliferate and migrate.
To confirm their observations that bacterial infections were directly facilitating the progression of cancer and helping the tumour escape the immune system, scientists infected colorectal cancer cells from a patient tumour and grew them in lab to form ball of cells called cancer spheroid—which mimics a tumour.
“In the presence of Fusobacterium, cancer cells increased their migration, so that they can move away from the central tumour,” Bullman says.
Bacterial infection also trapped neutrophils, the white blood cell that protect the body from infections, at the centre of the infected cancer spheroids. This would help the cancer cells escape the T cells, Bullman explains. In the presence of bacteria, the tumour cells also migrated as single cells, bringing bacteria with them. This was like Bullman’s previous study that showed that F. nucleatum often hitches rides with colorectal cancer metastases.
“Microbes in cancer cells are friends with benefits,” Johnston says. “There are interactions going on between microbes that are helping cancer cells to survive and progress towards states that are bad for the patient overall.” The bacteria not only help cancer cells evade the immune response, but they also break down or neutralise the chemotherapeutic drugs that are supposed to be killing the cancer cells, Johnston explains.
Bullman’s studies only include two tumour types and a small number of patients, but Wargo hopes that larger efforts will move findings from the lab into the clinic one day.
So far Bullman’s study shows that 15 percent of the 1,846 screened bioactive compounds that can kill F. nucleatum and other microbes also had potential as cancer chemotherapy drugs. That suggests that existing drugs can be reevaluated for their efficacy as both anticancer drugs and antimicrobial drugs— specifically targeting tumour-dwelling bacteria.
We can destroy or modulate these tumour-associated microbes, Bullman says, so the finding that bacteria within tumours are blocking the immune system from destroying cancer cells and helping the cancer spread “is actually very good news.”

Leave A Comment
You must be logged in to post a comment.