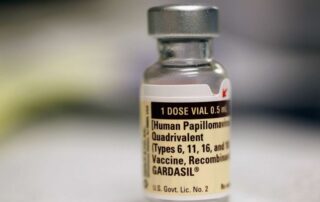
Achieving an 80% HPV vaccination rate could eliminate nearly 1 million cases of male oropharyngeal cancer this century
Source: medicalxpress.com Author: University of Texas Health Science Center at Houston A nationwide effort to adequately vaccinate 8 in 10 adolescents against the human papillomavirus (HPV) could prevent 934,000 cases of virus-associated, male oropharyngeal cancer over this century, reported investigators at The University of Texas Health Science Center at Houston (UTHealth Houston) School of Public Health in The Lancet Regional Health—Americas. At the start of each decade, the Healthy People program of the U.S. Department of Health and Human Services establishes goals to reduce the most significant preventable threats to health, which include an 80% target for the HPV vaccination program. However, in the U.S., just 54% of adolescents and only 21% of young adults were adequately vaccinated as of 2019. To gage the effect of accomplishing an 80% target on male oropharyngeal cancer, the most common cancer caused by HPV, UTHealth Houston researchers created a simulation model to project the development of this cancer over a lifetime and to measure the impact of the HPV vaccination. "Our study is the first to develop and validate a comprehensive mathematical modeling framework of the natural history of oral HPV infection and its progression to oropharyngeal cancer," said Ashish A. Deshmukh, Ph.D., MPH, the study's senior author and an associate professor in the Department of Management, Policy and Community Health and associate director of the Center for Health Services Research at UTHealth School of Public Health. "Achievement of the 80% goal by 2025 and maintaining it could lead to the prevention of [...]