Source: www.forbes.com
Author: Bruce Y. Lee

If a bill recently introduced in Florida passes, the human papillomavirus (HPV) vaccine would be mandatory for adolescents attending public school in the state. Currently, the vaccine is mandatory for boys and girls in Rhode Island and just girls in Virgina and Washington, DC. (AP Photo/John Amis, File)
Florida isn’t kidding about low human papillomavirus (HPV) vaccination rates. If you are a kid enrolled in a Florida public school, come July 1, 2018, you may be required to get the HPV vaccine. That is if you are old enough and if a bill now being debated in the Florida state legislature ends up passing.
If it gets through, Senate Bill 1558 would then become known as the “Women’s Cancer Prevention Act”, which is a much easier name to remember and also reflects some major benefits of the HPV vaccine. As the National Cancer Institute explains, HPV vaccine can help prevent not only cervical cancer but also many vaginal and vulvar cancers. In fact, two types of HPV (16 and 18) cause around 70% of cervical cancers. But just because you don’t have a vagina, cervix, and vulva doesn’t mean that you are in the clear. HPV is responsible for about 95% of anal cancers, 70% of oropharyngeal (the middle part of the throat) cancers, and 35% of penile cancers. Thus, the “Women’s Cancer Prevention Act” is really a “Cancer Prevention Act.”
Regardless, Florida State Senator José Javier Rodríguez (D-Miami) filed this bill on January 4 in an effort to boost Florida’s not so great HPV vaccination rates. According to the just-released Blue Cross Blue Shield Association (BCBSA) Health of America Report, only 29.0% of adolescents in Florida got the first dose of the HPV vaccine and only 7.3% got all doses in the series as of 2016. Those numbers are lower than the national average (34.4% got the first dose) but not the worst in the country.
New Jersey was the worst (not in general as a state but in terms of HPV vaccination rates). Based on the BCBSA report, as of 2016, only 20.6% of adolescents in New Jersey had gotten the HPV vaccine by age 13 and only 3.4% had completed the series. The Health of America report was the result of an analysis of medical claims data from 2010 through 2016 of over 1.3 million BCBSA commercially-insured adolescents across the country. The analysis considered vaccination to be on time if performed between the adolescent’s 10th and 13th birthdays, corresponding with the Centers for Disease Control and Prevention (CDC) recommendations of 11 to 12 year olds getting the vaccine.
Of course, the analysis did not include all adolescents in America. As BCBSA Chief Medical Officer Trent Haywood, MD, JD, explained, “the analysis represented the commercial population and didn’t include Medicaid populations. Also, to be included in the analysis, an adolescent had to be continuously enrolled with BCBS.” But studying such a large population is a pretty good shot at trying to figure what’s going on with shots and adolescents nationwide.
The report also showed that girls were better than boys (again, not in general, but in terms of HPV vaccination rates). In 2016, 37% of girls had received the first dose of the HPV vaccines by age 13 compared to 32%.
The best state of the bunch? Rhode Island with 57% of adolescents having received their first dose by age 13. Not coincidentally Rhode Island is the only state requiring HPV vaccine for both male and female students, starting with the first dose by 7th grade. Virginia and Washington, DC, have requirements just for females.
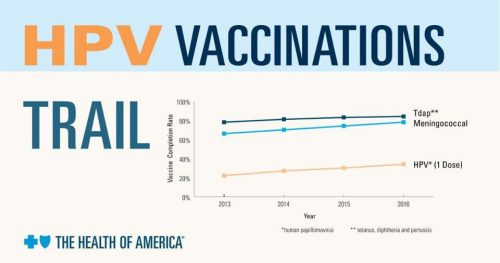
The good news is that nationwide vaccination rates steadily rose from 22% getting the first dose by age 13 in 2013 to 34% in 2016. But why are vaccination rates still well below 50% in most states? A BCBSA-commissioned survey of over 700 parents of adolescents aged 10-13 revealed the following top three reasons for parents not vaccinating their child against HPV:
- Being concerned about adverse side effects (59.4%)
- Not thinking their child is at risk (23.6%)
- Not knowing their child needed an HPV vaccination (15.7%)
Is requiring the HPV vaccine the solution? One argument against making the HPV vaccine mandatory is that people should be allowed freedom of choice. When Rhode Island first introduced its requirement, protests resulted various groups such as parents, a 2,400-member plus Facebook group, and the American Civil Liberties Union.
However, the counter-argument is that freedom of choice does not always hold when in the words of Spock, “the needs of the many outweigh the needs of the few.” You aren’t free to run up and down the aisle of an airplane naked and screaming because the needs of other on the plane outweigh the needs of you. Similarly, the HPV vaccine could help slow and even stop the transmission of HPV throughout the population, which can result in cancers that not only affect the cancer victims but also society by adding to health care costs.
Here is a Today show segment on the HPV vaccine:
Also, when a child doesn’t get vaccinated, it is usually because of the parent’s choice and not the child’s. Could making the vaccine mandatory in fact be protecting the child?
Another argument used by some is that the HPV vaccine has adverse effects. There are websites claiming that HPV vaccine can cause “crippling side effects” and “death.” But many of these scarier claims are not supported by rigorous scientific evidence. (Note: there are also websites that say that the Earth is flat, Elvis was an alien, and the government controls the weather). While nothing is completely safe (e.g., even a chocolate chip cookie in the right situation could do some real damage) and all vaccines do have their risks, the risks of the HPV vaccine are comparatively very low and far outweighed by the potential benefits as indicated by the CDC.
As I wrote before for Forbes, some have argued that the HPV vaccine is a “gateway to sex” and thus making it mandatory would increase the number of teenagers having sex and encourage promiscuity. However, this goes counter to the recent trend of teenagers delaying when they first have sex and suggests that teenagers would not have sex if it weren’t for that darn HPV vaccine. A related argument is that the HPV vaccine would give teens a false sense of security that they are protected against all sexually transmitted infections, leading them to not practice safe sex. However, raising awareness of what the HPV vaccine actually does could help overcome this concern.
All of this does not necessarily mean that making HPV vaccination mandatory is the solution. However, what then is the solution to a majority of adolescents still not getting vaccinated (at least by age 13 and when sexual activity for some begin)? As Haywood described, this is a situation in which many are “not taking full advantage of preventive measures. A big issue is lack of awareness of the HPV vaccine and its benefits.” HPV vaccine awareness campaigns may help push up vaccination rates, but by how much?
The wonderfully straight-forward and transparent world of politics will help determine whether Senate Bill 1558 becomes a law in Florida. A similar bill failed to pass in 2011. But things have changed since 2011, in good ways and bad.

Leave A Comment
You must be logged in to post a comment.