Source: www.bbc.com
Author: Natalie Grice, BBC News
“A patient once described it to me as brutal, and it’s really stuck with me, because it’s difficult to go through.”
What’s so brutal?
It’s the cancer treatment Prof Mererid Evans routinely prescribes to the people who come to her, hoping she will save their lives, and which she aims to improve with research she is leading.
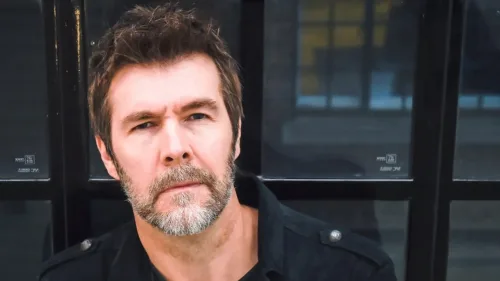
It was the same word used by Welsh comedian Rhod Gilbert when in 2022 he found himself sitting in front of the consultant oncologist after being diagnosed with throat, neck, tongue and tonsil cancer.
Her famous patient suddenly put her consulting room at Velindre Cancer Centre, Cardiff, in the limelight when he made a documentary about his treatment.
“Rhod wanted something positive to come out of his experience,” said Prof Evans, 54, head and neck specialist at Velindre Cancer Centre in Cardiff, a professor at Cardiff University’s cancer and genetics division, and head of the Wales Cancer Research Centre.
“We talked about the treatment he’d be receiving and I think he felt it was an opportunity to highlight what it’s like going through cancer treatment.”
The resulting Channel 4 programme, A Pain in the Neck for SU2C, followed Gilbert through diagnosis, treatment and the aftermath.
Head and neck cancer is the eighth most common form of cancer overall in the UK, although it is two to three times more common in men, for whom it is the fourth most likely form.
About 12,500 new cases are diagnosed each year, according to Cancer Research UK, and incidences are on the rise. About 4,000 people die from it annually.
Prof Evans discovered the comedian’s treatment was to be filmed a few days before it began.
“I don’t think he knew before he started how impactful him recording his journey would be. I think it was something that he wanted to do for himself because this is what he does,” she added.
“And he felt he could turn something that was a very difficult experience into a positive.
“I think that that’s how he’s reflected on having done it, that it’s raised a lot of awareness and hopefully has helped people in a similar situation to him.”
Prof Evans tried to carry on as normal in her interactions during their consultations, despite having a film crew present.
Gilbert was treated with radiotherapy and chemotherapy, which Prof Evans called “particularly difficult” for head and neck cancer.
“When you have a tumour or cancer in the back of your throat, either in the tonsil or the back of the tongue or the roof of the mouth, when you try and treat that with radiotherapy, what effectively you are causing is big ulcers in the patient’s mouth and throat that get worse over a six-week period,” she added.
“The side effects are a dry mouth, lack of taste, ulcers that make swallowing very painful and difficult and sometimes requires feeding through a tube in the tummy as we saw [happen to him] in the documentary.”
It also causes fatigue which can take months to get over, she added, and the effects are compounded if a patient also has chemotherapy, which can cause nausea, vomiting and infections.
Another particularly significant side effect for a performer is changes to the voice.
“Radiotherapy to the head and neck does cause some swelling and inflammation within the voicebox,” she explained.
“It’s not uncommon that people develop a hoarse voice during treatment, and that doesn’t always improve. So that was a real fear, and that was clearly a big one for someone who makes their living by using their voice.”
This was echoed by Gilbert in the programme.
One of the first things he said was: “I’m worried that the radiotherapy might seriously knacker my voice. I’m a stand-up, so this treatment could save my life, but kill my career.”
He was eventually given the all-clear.
Which cancers does HPV cause?
Gilbert’s cancer was caused by the human papilloma virus (HPV), more commonly associated with cervical cancer.
A programme of vaccination for girls against HPV to tackle cervical cancer, given at the age or 12 or 13, was introduced in 2008.
Prof Evans was involved in two studies looking at the prevalence of HPV cancers in men which were used as evidence for the Joint Committee on Vaccination and Immunisation to subsequently extend the HPV vaccine to boys in 2019, which was “very rewarding to see”.
The HPV vaccination programme in girls has seen a near 90% reduction in cervical cancer rates in girls who were first vaccinated at 12 or 13, and a 97% reduction in pre-cancerous cell changes that can lead to cervical cancer.
“If HPV vaccine were given to everyone, one would imagine the rates should come down to virtually zero,” she said.
“The issue is making sure vaccination rates are high and that they’re maintained so that transmission within the population is broken, but it’s going to take a long time.
“In the meantime, we’re going to see large numbers of people who have HPV-related cancers and we need to treat them.”
Part of her work now is leading a trial, along with Prof Terry Jones from Liverpool University, looking at gentler treatments that will be as effective.
The trial, known as Pathos, is using minimally invasive surgery carried out by robotic or laser methods, and lower doses of chemotherapy or radiotherapy.
Seeing how the patient copes with treatment outside hospital was a benefit of the documentary, Prof Evans believes.
She said: “I think it was incredibly brave of him to open up and show honestly what the experience was like for him. It wasn’t just the physical, it was the emotional and mental challenge that treatment was for him to get through.
“We don’t often see that side of somebody’s journey because when they come to clinic we talk about very practical things like ‘how’s your swallowing? How’s your pain? Are you using the mouthwashes?’
“Often it isn’t a space where we see the reality of living with something every minute of every day, every hour of every day when it is very, very difficult.”



Leave A Comment
You must be logged in to post a comment.