Source: www.eurekalert.org
Author: Mass General Brigham
Researchers develop innovative technique for distinguishing tumor from normal tissue
The visual and quantitative techniques used – including high-speed cameras to detect changes occurring in a billionth of a second – had an accuracy of 97% across tumor types (liver, brain, tongue, skin, breast, bone and soft tissue)
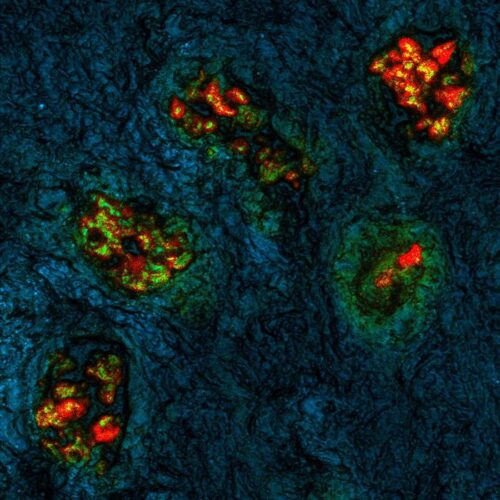
The images show clusters of colorectal cells metastasized to the liver, resected from a patient at Massachusetts General Hospital (MGH) The cells are visible as red, which means longer lifetime, against a background of normal liver tissue in blue/green
- Mass General Brigham investigators tested their approach using specimens from multiple cancer types, including liver, brain, tongue, skin, breast, bone and soft tissue
- Their visual and quantitative technique, which combines an injected FDA-approved drug with high-speed cameras to detect changes occurring in a billionth of a second, had an accuracy of 97% across tumor types
Removing a patient’s tumor while sparing healthy tissue requires exquisite precision, but often surgeons must rely on their eyes and hands to determine where to cut. A team led by researchers from Mass General Brigham has developed a visualization tool that combines high-speed cameras and fluorescent injection to distinguish tumor tissue from normal tissue across cancer types. The team evaluated the new imaging technology, known as fluorescence lifetime (FLT) imaging, using specimens from more than 60 patients that underwent surgery of various cancers. In a paper published in Nature Biomedical Engineering, the team reported that the technique was over 97 percent accurate across tumor types, with the potential to improve the accuracy of cancer surgeries.
“This collaboration has been thrilling,” said corresponding author Anand Kumar, PhD, of the Athinoula A. Martinos Center for Biomedical Imaging at Massachusetts General Hospital (MGH). “Our lab has been studying fluorescence lifetime imaging since 2002, but this is the first time that anyone has combined it with tumor imaging and injectable dyes in humans. By doing so, we’ve developed a technique for accurately distinguishing tumor tissue from healthy tissue across cancer types.”
Kumar worked closely with colleagues at Mass Eye and Ear, another member of the Mass General Brigham healthcare system, where patients are treated for head and neck cancer.
“This technology has taken us to the brink of a revolution in solid tumor surgery,” said Mark Varvares, MD, chief of Otolaryngology–Head and Neck Surgery at Mass Eye and Ear. “By using the advanced imaging techniques combined with the dye, surgeons in the near future will have the ability to more completely remove all malignant cells during tumor surgery while at the same time, with confidence, spare normal tissue, enhancing postoperative function and in some cases, the patient’s appearance.”
Mass General Brigham brings together 16 member institutions, including academic medical centers, top-tier specialty hospitals, community hospitals, a rehabilitation network and more. Research that spans more than one of these entities is more than the sum of its parts, helping to provide insights and unique perspectives from multiple settings and areas of expertise.
Many technologies have been pursued to improve visualization of tumors during surgery, including fluorescence imaging and advanced microscopy, but such technologies have not yet been widely adopted and most are restricted to specific types or subtypes of cancer. Fluorescence imaging can use dyes to target cancer-specific molecules, but standard imaging techniques can have limited accuracy for detecting tumor margins—or the edges of normal tissue that surround a tumor—since the expression of these molecules can vary widely within and across tumor types.
The technique used by Kumar and colleagues, known as FLT imaging, takes a different tact. Instead of relying on dyes only for targeting cancer, the technique uses high-speed cameras to detect changes in the property of the light emitted by tissue. In previous studies in preclinical models, Kumar and colleagues found that tumors in mice injected with a dye known as indocyanine green (ICG) had a longer fluorescence lifetime compared to normal tissue. This difference allowed the researchers to accurately distinguish between tumor tissue and normal tissue.
In their current study, the team applied the same principle to samples from patients. The team began by analyzing samples from patients undergoing liver surgery at MGH and head and neck surgery at Mass Eye and Ear. Patients had received an ICG injection at least a day before the surgery.
Building on this initial work, the team collaborated across multiple institutions and evaluated specimens from more than 60 patients representing multiple cancer types, including liver, brain, tongue, skin, bone and soft tissue, who were treated at MGH, Mass Eye and Ear, The University of Pennsylvania, University of Newcastle in the UK, and Leiden University in the Netherlands.
The team was able to detect an FLT shift at the cellular level that was consistent across tumor types and in multiple patients. The technique was also able to distinguish benign from metastatic lymph nodes. Overall, it was more than 97 percent accurate at distinguishing tumor tissue from healthy tissue.
The authors note that although ICG is approved by the Food and Drug Administration for other indications, it is not yet approved for clinical use as a tumor marking agent. The researchers’ next step is to perform a larger scale clinical trial to test the safety and efficacy of fluorescence lifetime imaging with ICG for tumor identification during surgeries.
“Our work suggests that the combination of fluorescence lifetime imaging with ICG could improve surgical resections, thereby impacting patient lives,” said Kumar. “We’re excited to take these next steps to move our discoveries closer to clinical impact.”
Notes:
Authorship: Mass General Brigham co-authors include Rahul Pal (MGH), Murali Krishnamoorthy (MGH), Hannah R. Collins (MGH), Shriya Shukla (MGH), Amy L. Kendall, Michael S. Marshal (MGH), Stefan A. Carp (MGH), Yin P. Hung (MGH), Angela R. Shih (MGH), Maria Martinez-Lage (MGH), Lawrence Zukerberg (MGH), Peter M. Sadow (MGH and Mass Eye and Ear), William C. Faquin (MGH and Mass Eye and Ear), Brian V. Nahed (MGH), Allen L. Feng (Mass Eye and Ear), Kevin S. Emerick (Mass Eye and Ear), Santiago Lozano-Calderon (MGH), Mark A. Varvares (Mass Eye and Ear), and Kenneth K. Tanabe (MGH). Additional co-authors include Thinzar M. Lwin, Corey D. Chan, Andrey Prilutskiy, MacLean P. Nasrallah, Tom H. Dijkhuis, J Sven D Mieog, Alexander L. Vahrmeijer, Karthik Rajasekaran, John Y. K. Lee, and Kenneth S. Rankin.
Disclosures: Kumar, Krishnamoorthy and Pal are co-inventors of a pending U.S. Patent application issued to The General Hospital Corporation. The patent might be the subject of a licensing agreement in the future. Hung received royalties from Elsevier publishing company unrelated to this study. Rankin received remuneration for lecturing on a Stryker Fluorescence Guided Surgery Conference.
Funding: This work was supported in part by the National Institutes of Health (R01-CA211084, R01-CA260857, 1P01CA240239) and the MGH-Executive Committee on Research Interim Support Fund.
Paper cited: Pal R et al. “Fluorescence lifetime of injected indocyanine green as a universal marker of solid tumours in patients” Nature Biomedical Engineering DOI: 10.1038/s41551-023-01105-2

Leave A Comment
You must be logged in to post a comment.