Source: nurse-practitioners-and-physician-assistants.advanceweb.com
Author: Amber Crossley, MSN, ARNP, FNP-BC
Oral carcinoma is identified as one of the top ten cancers worldwide, accounting for nearly 2% to 5% of all cancer cases.1, 2 In 2014, there were an estimated 42,440 new cases of oral and pharyngeal carcinoma.
Males have a greater risk of developing the disease compared to females.2 Black males in particular are amongst the highest at-risk group for developing oral carcinoma.2 Oral carcinoma typically develops after the age of 50, with the majority of cases occurring between the ages of 60 and 70.2 When initially diagnosed with oral carcinoma, more than 50% of people will have metastases.3
The most common causes of oral carcinoma are related to tobacco use and alcohol consumption.4 In fact, 75% of all cases of oral carcinoma may be caused by the combination of tobacco and alcohol use.4
However, it has also been extrapolated that chronic trauma to the oral mucosa, such as in the case of ill-fitting dentures or the consumption of high-temperature foods, is a leading modifiable risk factor for oral carcinoma.1,5 Dietary deficiencies of vitamins A, C, E, selenium, and folates may also contribute to the development of malignant cancerous lesions in the oral cavity.6
While cases of oral carcinoma have decreased over the last few years in the United States, oropharyngeal cancer is increasing in incidence.4 The rise in cases of oropharyngeal cancer may be related to viral and infectious diseases; however, the mechanisms are largely unclear. Some of these infections and viruses include human papilloma virus (HPV), periodontitis, candida albicans, syphilis and herpes simplex virus.7 However, for the purposes of this case presentation, only oral cavity cancer will be discussed.
A Non-Healing Oral Lesion
MC is an 82-year-old white female who visited her primary care provider’s office complaining of a mouth sore. The sore was present for approximately six months, and grew increasingly painful.
She has worn dentures for more than 10 years, and was accustomed to the typical soreness with irritation sometimes associated with everyday denture use. With this particular occurrence, the soreness lingered in the same area and lasted longer than any previous experience.
MC attempted to alleviate the soreness with an existing prescription for hydrocodone. This treatment proved unsuccessful. MC scheduled an appointment with her primary care provider, as she assumed the pain was the result of ill-fitting dentures.
At MC’s initial appointment, the provider noticed a 7mm erythematous lesion on the lower interior aspect of her right molar, and suggested it could be the result of her ill-fitting dentures. Because MC had exhausted her hydrocodone, the provider prescribed tramadol and a viscous lidocaine suspension for pain. She was told to follow-up with her dentist once the sore completely healed in order to be fitted with new dentures. She was instructed to refrain from denture use until the sore had resolved. There were no further follow-up instructions given.
One week after the initial visit, MC returned to the primary care provider’s office because of increasing pain and discomfort. During this visit, the provider noted the sore had ulcerated edges that were friable and showed little improvement. She was referred immediately to an otolaryngologist for the suspicion of carcinoma of the oral cavity.
Patient History
MC is an 82-year-old widow. She is a Medicare recipient living in government-subsidized housing for the elderly. MC smoked tobacco between the ages of 17 and 52 at a rate of 1.5 packs per day, or 53 pack years. During the same 35 year time frame, she drank 1 to 2 alcoholic beverages daily.
Over the past 10 years, she lost a total of 40 pounds without any lifestyle modifications to justify the weight loss. At the time of MC’s initial primary care visit, she weighed 91 pounds. Additional patient history included hypothyroidism, mitral stenosis, gastroesophageal reflux disease, coronary artery disease, arthritis and hypertension.
Clinical Features
Oral carcinoma is defined as cancer involving the floor of the mouth, hard palate, buccal mucosa, interior tongue, retromolar trigone, or alveolar ridge.8 Premalignant oral carcinoma may present as a painless white patch known as leukoplakia, or a painful reddened patch identified as erythroplakia.9 In addition to the aforementioned signs, the cervical lymph nodes may be enlarged.10 Any erythroplakia or leukoplakia lesions that appear to be non-healing in an older individual should be deemed suspicious.10
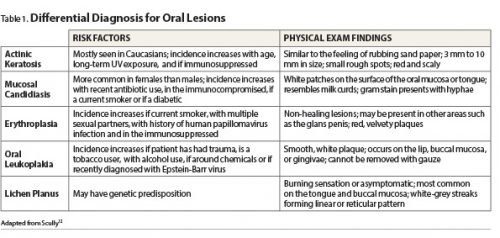
Differential Diagnosis
Refer to the table below to help you rule out other conditions.
Diagnosis
Early identification of oral carcinoma offers patients the greatest chance for successful treatment and survival following diagnosis.5
An initial patient history that includes tobacco use, alcohol consumption, sexual practices, denture use, oral trauma, infections of the oral cavity and a history of present illness should be obtained.8 It is important to understand that patients complaining of ill-fitting dentures are four times more likely to develop an oral lesion that is cancerous.5
Oral lesions caused by trauma increase the likelihood of carcinogen absorption from tobacco and alcohol in the oral mucosa. This absorption may disrupt the deoxyribonucleic acid of the mucosal cells.1
Following a thorough history, the provider can perform a complete head and neck examination. During oral cavity inspection, a mirror and fiberoptic exam should also be performed.8 A combination of inspection and palpation for lumps or abnormalities within the tissue of the oral mucosa is the definitive mechanism used to screen for oral cancer as identified by the U.S. Preventive Services Task Force.4 In the presence of a potentially cancerous oral lesion, a surgical biopsy should be completed to confirm a diagnosis of oral carcinoma.9
Imaging studies can be used to detect and identify metastases of oral carcinoma. Computed tomography is the preferred imaging study performed at the site of the primary tumor.11 This study can identify the extent of the tumor, as well as lymph node involvement.10,12 Additionally, a chest x-ray is recommended in order to determine whether or not the oral carcinoma originated in the lungs or metastasized to the lungs. The lungs are the primary site for metastases of oral carcinoma.12 More than 90% of oral cavity cancers are considered to be squamous cell carcinoma.11
Laboratory studies should also be considered in addition to imaging studies. Serum ferritin, alpha anti-trypsin, and alpha-antiglycoprotein levels can be elevated in patients with advanced cancer of the head or neck region.12 Laboratory studies alone cannot determine the presence of oral carcinoma. However, they can aide in identifying the extent and progression of the cancer.12
Case Outcome
A surgical biopsy was performed in order to identify the causative organism. MC was diagnosed with stage IV malignant squamous cell carcinoma of the right retromolar trigone, as well as squamous cell carcinoma of the right middle and lower lobe of the lung. The patient had no lymph node involvement.
Because of her increased age and nutritional status, MC did not qualify for multimodal treatment. Instead, she is being treated with aggressive radiation therapy over a period of 12 weeks.
Understanding key factors related to MC’s case — increased age, history of tobacco and alcohol use, and ill-fitting dentures — is paramount when identifying the painful, non-healing, 7 mm lesion in her oral cavity as a potential diagnosis of oral carcinoma.
Implications for Practice
Due to the increase in oral health disparities, the Institute of Medicine released a report revealing a new demand for non-dental health care providers to perform screenings for oral diseases as well as offering prevention advice and referral to preventative services.13
Increasing interprofessional collaboration amongst dentists, nurse practitioners, physician assistants, physicians and medical students has shown to be effective in implementing the head, ears, eyes, nose, oral cavity, and throat (HEENOT) assessment into practice.14 While this is similar to the head, ears, eyes, nose and throat assessment, it allows for the integration of the oral cavity into the evaluation of the head and neck exam.
One study, conducted between 2008 and 2014 at New York University, revealed that the result of HEENOT implementation led to 500 patient referrals to dental clinics for suspicious oral lesions.14 Preventative measures at the primary care level should focus on the greatest risk factors (tobacco use, alcohol consumption and ill-fitting dentures).
Research has shown that due to the sometimes vague and misleading symptoms of early-onset oral carcinoma, a diagnosis may be prolonged by up to 6 months.12 Although screening for oral cancer in healthy individuals without risk factors may not be beneficial, evidence supports oral screenings by primary care providers for high-risk patients.3, 4, 15
Given the fact that only 30% of patients ages 65 years and older have dental insurance coverage, the primary care provider must screen patients who present with many risk factors for oral carcinoma.14,16 Because there are a greater number of primary care providers in comparison to dentists, they have the potential to increase awareness and detection of oral carcinoma.16
While the leading cause for oral carcinoma is tobacco use, it is recommended that the primary care provider encourage patients who use tobacco to employ smoking cessation products.4 Second, the primary care provider should educate patients on the harmful effects of daily alcohol use.12 Third, providers should stress to patients the importance of regular dental check-ups and denture fittings as an essential tool for maintaining good oral health.5
Note:
Amber Crossley practices as an advanced registered nurse practitioner in Jacksonville, Florida.
References
1. Piemonte ED, et al. Relationship between chronic trauma or the oral mucosa, oral potentially malignant disorders and oral cancer. J Oral Pathol Med. 2010;39(7):513-517.
2. National Cancer Institute. Stat fact sheets: oral cavity and pharynx cancer. http://seer.cancer.gov/statfacts/html/oralcav.html.
3. Rethman MP, et al. Evidence-based clinical recommendations regarding screening for oral squamous cell carcinoma. JADA. 2010;141(5):509-520.
4. U.S. Preventative Services Task Force. Oral cancer: screening. http://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/oral-cancer-screening1
5. Manoharan S, et al. Ill-fitting dentures and oral cancer: a meta-analysis. Oral Oncol. 2014;50(11):1058-1061.
6. Freedman ND, et al. Fruit and vegetable intake and head and neck cancer risk in a large United States prospective cohort study. Int J Cancer. 2008;122(1):2330-2336.
7. Meurman JH. Infectious and dietary risk factors of oral cancer. Oral Oncol. 2010;46(6):411-413.
8. National Comprehensive Cancer Network. Head and neck cancers. http://oralcancerfoundation.org/treatment/pdf/head-and-neck.pdf
9. Jefferson GD. Adult with oral cavity lesion. AAO-HNSF Patient Month Program. 2011;40(5): 1-25.
10. Arya S, et al. Head and neck symposium: imaging in oral cancers. Indian J Radiol Imaging. 2012.22(3):195-208.
11. Akram S, et al. Emerging patterns in clinico-pathological spectrum of oral cancers. Pak J Med Sci. 2013;29(3):783-787.
12. Scully C. Cancers of the oral mucosa. Medscape. 2016. http://emedicine.medscape.com/article/1075729-overview
13. Institute of Medicine. Improving access to oral health care for vulnerable and underserved populations. https://www.iom.edu/Reports/2011/Improving-Access-to-Oral-Health-Care-for-Vulnerable-and-Underserved-Populations/Report-Brief.aspx.
14. Haber JH, et al. Putting the mouth back in the head: HEENT to HEENOT. Am J Public Health. 2015;105(3):437-441.
15. American Family Physician. Screening for the early detection and prevention of oral cancer. http://www.aafp.org/afp/2011/0501/p1047.html
16. Cohon LA. Expanding the physician’s role in addressing the oral health of adults. Am J Public Health. 2013;103(3);408-412.


Leave A Comment
You must be logged in to post a comment.