Source: www.rdhmag.com
Author: Nancy W. Burkhart, RDH, EdD
Patients are sometimes followed for periods of time for what is called dysplasia, leukoplakia, keratotic lesions, and previous frank carcinoma. With any degree of tissue change, the person should be followed closely and an etiology always needs to be determined. Sometimes, removal of a frictional component is suggested; at other times, the lesion may have a more ominous appearance that will alert the clinician that cancer might be high on the differential list. Obviously, in highly suspicious lesions, a biopsy would occur immediately.
Patients will sometimes tell the clinician that they were previously biopsied and the report will note “evidence of dysplasia.” Sometimes a diagnosis is made of dysplasia, but the lesion becomes carcinoma over time, even after the initial removal of the lesion. The reverse may be true as well, where the body responds physically and the tissue regains a state of health.
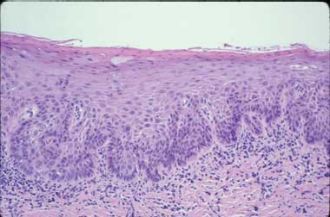
Figure 1: This image depicts moderate dysplasia, displaying increasing cytologic atypia and alteration of maturation in the lower half of the epithelium. Courtesy of Dr. John Wright, From General and Oral Pathology for the Dental Hygienist. Lippincott Williams & Wilkins, 2008
Why does one individual develop carcinoma while another person may develop a mild epithelial dysplasia? Perhaps the body is able to stop progression or reverse the state of progression. These are questions that researchers continue to evaluate and study.
Frictional keratosis, though, is not in the same category as dysplasia. When the frictional component is removed, the lesion will subside. An example of a common lesion that has a frictional component is cheek chewing or morsicatio buccarum. However, chronic frictional or chemical assault on the tissue over time can also cause dysplastic changes.
The body has the miraculous ability to repair damage caused by our environment and lifestyle factors. We are discovering, for example, the role that our food plays in reducing cancer risks and even altering our susceptibility toward genetic factors. Our mental, physical, and spiritual make-up will play a very strong role in individual disease states, as well as during recovery. Researchers are now discovering that the very food we place in our bodies has great healing powers and may prevent many known diseases while promoting total health. Along the same lines, exposure to environmental agents has been documented as having profound effects on our bodies as well.
The factors that allow an oral pathologist to diagnose a tissue specimen as dysplastic (see Figure 1) are the following (Wright J, 2008):
An increase in cellular nuclear/cytoplasmic ratio
Rounded rete ridges often described as “saw-tooth” in appearance
Noticeable maturation
Evident mitosis with atypical findings, as well as mitosis in upper layers of the epithelium
Visible changes in pleomorphism in the cell size as well as the shape of individual cells
Dark, staining cells are visible –nuclear hyperchromatism
Nucleoli are enlarged and appear darkly stained
Cellular adhesion is lost
Abnormal keratinization patterns arise
All of the features will vary with individual tissue specimens, and the degree to which the dysplasia is classified may vary with pathologists viewing the same tissue specimen. Generally, three classifications occur – mild dysplasia, moderate dysplasia, and severe dysplasia.
If the tissue is not treated surgically or ablated with laser surgery, carcinoma in situ or frank squamous cell carcinoma will likely result. Any contributing lifestyle such as alcohol or tobacco use may lead to the progression of dysplasia and should be discontinued. As progression continues, invasion of the transformed cells to the tissue below the basement membrane will occur and the designation of invasive carcinoma is evident.
The importance of the oral exam, including both the extraoral and intraoral, cannot be emphasized enough. Despite the newest techniques with lights, rinses, and various tests, the gold standard in any unexplained finding, when an etiology cannot be found, is to biopsy for microscopic confirmation. Some lesions cannot be seen – especially those in the most posterior regions and the tonsils/tonsillar crypts – and palpation along with careful visual screening is a key factor.
The dilemma occurs when a suspicious area has no known cause and the decision rests on whether to biopsy at that time, follow the area, or use one of the available adjunct devices for more information. All adjuncts that can be used are just that – adjuncts. Nothing takes the place of a thorough intraoral and extraoral exam when performed correctly. With all of the information available, the clinician must decide along with the patient what the optimal choice must be at that time. The choices would be to proceed with a referral, perform a biopsy, or monitor the lesion.
A recent editorial written by Dr. Mark Lingen, editor-in-chief, of Oral Surgery, Oral Medicine, Oral Pathlogy, Oral Radiology, and Endodontology, emphasized the need for dental education in head and neck screening for squamous cell carcinoma. With an annual incidence worldwide of more than 500,000 cases, it is the sixth most common malignancy. Dr. Lingen praised the efforts of the American Academy of Oral Medicine and the Academy of Oral and Maxillofacial Pathology for their continued focus on educating dental students in performing the head and neck exam. He applauded the efforts put forth by the American Dental Association’s Commission on Dental Accreditation to require that dental students be proficient in the oral cancer exam during school and as a proficiency exam by graduation. He also asked some good questions about how these efforts will be carried out and how the students will be assessed long-term.
The editorial speaks to the question of how will schools ensure that their own faculties are proficient as well in the dental exam in order to teach the students. Dr. Lingen cites several research studies in the past few years that suggest the graduating dental students and practitioners do not feel comfortable with the dental exam in detecting head and neck cancer and that they feel inadequately prepared. He also emphasizes the need for continuation of pathology and dental exam skills during all the years that a dental student spends in school.
Over the years, I have corresponded with thousands of patients who have contacted me through The International Oral Lichen Planus Support Group (founded in 1997). I have heard more times than I want to mention that “the dental office really never checks my lichen planus and they just tell me to learn to live with it – it is only lichen planus.”
We hear so many times from patients who have long-term oral lesions – lichen planus, ulcerative disease states, and even long-term undiagnosed lesions – and somewhere along the way the tissue became dysplasia or ultimately oral cancer. Any lesion needs to have a diagnosis, and long-standing disease states need to be carefully monitored at frequent intervals. Long-term inflammation anywhere in the body is detrimental. Even previous dysplasia and cancer should be followed carefully because of potential recurrence. The concept of “field carcinogenesis” means that other malignancy may occur from new foci and cell transformation related to the previous lesion.
We have heard from family members who tell us that the person who corresponded with us has died, but they are contacting us to say thank you for trying to help even though it was too late.
Often, it is the person who is undergoing surgery with radiation treatment who emails me to update me on their progress.
Emotional support is time-consuming but greatly needed and freely given. Busy offices are usually pressed for time, but answering questions, following up with patients, and offering your concern is part of a healing process. It is truly sad that so much emphasis is placed on cosmetic procedures, yet there is so little time for a good oral exam in the office. I think that hygienists need to make the oral exam a prime focus in their practices for every patient and at every visit.
If you do not feel confident in your own abilities with the oral exam, search for a CE course in your region to update your skills. No one is so knowledgeable that they cannot use a little more updating and education to make themselves a better healthcare provider.
Life is an ongoing educational process, no matter what aspect we are addressing. Education by its very nature is never wasted time.
As an educator, I feel strongly that continuing education is needed for key areas such as oral pathology and oral medicine – not only in dental schools but in offices as well. We are primary healthcare providers who can tell so much about a person by just performing a good intraoral and extraoral exam. With an aging population, an increase in oral cancer for those under 40 years of age, and even children developing oral disease states not usually found in the past, we need to concentrate on what is truly important. Update your skills and start sharing your expertise in helping others!
Keep listening to your patients and always ask good questions!
Notes:
1. Nancy W. Burkhart, BSDH, EdD, is an adjunct associate professor in the department of periodontics, Baylor College of Dentistry and the Texas A & M Health Science Center, Dallas. Dr. Burkhart is founder and co-host of the International Oral Lichen Planus Support Group (http://bcdwp.web.tamhsc.edu/iolpdallas/) and co-author of General and Oral Pathology for the Dental Hygienist. Her website for seminars is www.nancywburkhart.com.
References
1.Cannick GF, Horowitz AM, Drury TF, Reed SG, Day TA. Assessing oral cancer awareness among dental students in South Carolina. J Am Dent Assoc 2005;136:373-8.
2. Kahn M. Adjunctive Oral Premalignant Screening Devices-Clinical Protocol #12. From: DeLong L, Burkhart NW. General and Oral Pathology for the Dental Hygienist. Lippincott, Williams & Wilkins. Baltimore, 2008.
3. Lingen M. Assuring dental student head and neck cancer screening competency. Editorial in Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;111:3,267-68.
4. Pannone G, Santoro A, Papagerakis S, Lo Muzio L, De Rosa G, Bufo P. The role of human papillomavirus in the pathogenesis of head and neck squamous cell carcinoma: an overview. Infect Agent Cancer2011;Mar 29:6:4.
5. Siegel M, Murrah V, Aloise D. Head, Neck and Oral Cancer Examination. MedEdPORTAL; 2009. Available from: http://services.aamc.org/30/mededportal/servlet/s/segment/mededportal/?subid=7768.

Leave A Comment
You must be logged in to post a comment.