Source: Dr.Biscuspid.com
By Donna Domino, Features Editor
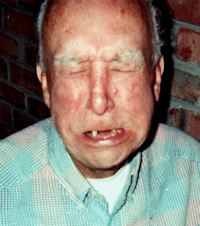
November 6, 2012 — Hank Grass has so far successfully fought his submandibular cancer. But the retired policeman is now facing bankruptcy in his losing battle to get Medicare to cover the oral surgeries, dental treatments, and dentures he needs following radiation treatment.
The 77-year-old had his salivary gland removed after doctors found cancer at the base of his tongue three years ago. But the radiation and chemotherapy damaged his teeth and gums so much that he had to have all but three of his bottom teeth extracted. Recently, Grass needed periodontal surgery to treat an infection he developed in his mandible from radiation treatments.
So far, Grass has spent $8,000 for the dental treatment and dentures, but Medicare won’t reimburse him, saying his dental work was not medically necessary and is cosmetic. And since Medicare has refused payment, Grass’ insurance company also has refused to cover the dental procedures.
“I’ve been through a living hell,” he told DrBicuspid.com. “We’re pinching pennies; we’re in bankruptcy.”
Five doctors — including his dentist, oncologist, oral surgeon, and the doctor who administered chemotherapy — submitted letters confirming that Grass’ dental procedures were directly related to his cancer treatments. But it was to no avail, he said.
“You don’t have to be a rocket scientist to look at all the letters from five doctors to figure out this is not cosmetic,” he asserted. “Of course it’s a result of my oral cancer. But they’ve got a thing they look at on a chart that classifies this as dental, but that’s a lot of baloney.”
When he tried to appeal, Grass said he was given the bureaucratic run around.
“We have tons and tons of paperwork that we sent over and over to Medicare,” he said. “It seems they try to exhaust you to the point that you give up. First they said we had 100 days to file an appeal. The next thing they turn around and say you’re late on your appeal. So one hand does not know what the other hand is doing. It’s such a pathetic situation.”
‘They hide behind rules’
Medicare policy, which excludes coverage of “routine” dental care, does cover dental services when they are “incident to and an integral part of” eligible medical care. Dental procedures that are covered include extractions in preparation of radiation treatment of neoplastic disease, reconstruction of ridges that are performed simultaneously with the surgical removal of oral tumors, and the wiring of teeth if done in connection with jaw fractures.
“I’ve been through a living hell. We’re pinching pennies; we’re in bankruptcy.”
Brady Semmel, DMD, a Wilmington, NC, oral and maxillofacial surgeon who performed Grass’ recent surgery, called his long-term dental prognosis “very poor.”
“Upon surgical exploration of the anterior mandible, I found dead, loose bone that had gotten infected,” Dr. Semmel told DrBicuspid.com. “This osteoradionecrosis is most likely due to the radiation treatment, and he is still at high risk for developing further areas of dead bone.”
He noted that, historically, Medicare has not covered procedures related to the teeth.
“It can be very difficult dealing with Medicare,” Dr. Semmel said. “I don’t think they will change things, but they probably should.”
Grass is not his only patient in the same situation. “I have a lot of patients that have dental problems that are related to their medical condition,” Dr. Semmel noted.
Medicare’s refusal to cover dental care stemming from underlying medical conditions is unfair, Dr. Semmel said.
“If a patient has a cancer resection of an area on the face and a part of the face is removed (for example, a nose), Medicare will pay for a prosthesis to replace the nose,” he noted. “But if you lose your teeth due to cancer, Medicare will not pay for a denture to replace the teeth.”
“They know this policy is wrong, but they hide behind the rules,” Grass said. “They look for the tiniest loopholes to make you stop.”
Federal lawsuit
Medicare’s refusal to cover extensive dental treatment that is often needed to treat patients with diseases such as oral cancer and Sjögren’s syndrome is unreasonable and arbitrary, according to a lawsuit pending in U.S. federal court.

The litigation, originally filed in 2008 on behalf of one plaintiff, was amended by the Center for Medicare Advocacy (CMA) in the U.S. District Court for the District of Arizona against U.S. Health and Human Services Secretary Kathleen Sebelius on behalf of three Medicare beneficiaries who needed medically related dental care stemming from underlying medical conditions.
Each of the plaintiffs in the CMA lawsuit suffered a serious medical condition, resulting in impairment of salivary gland function, with resulting damage to the mouth and teeth that threatened their overall health, according to the complaint.
But in each case they were denied coverage, for reasons ranging from “Medicare does not cover most dental services” to “when an excluded dental service is the primary procedure involved, coverage is excluded regardless of the complexity of the procedure.”
One of the plaintiffs, Ron Fournier, developed squamous cell cancer in his tonsils that metastasized to his neck nodes. His chemotherapy and radiation treatments resulted in mucositis, altered salivary gland function, and dental infections. He has extensive caries, and his teeth have broken off at gum level, leaving him unable to eat solid food, according to the complaint.
CMS did not respond to calls for comment on Grass’ case.
“Medicare has dodged this bullet for a long time, and it must be addressed,” said James Sciubba, DMD, PhD, an oral pathologist in Baltimore who is vice president of the advocacy group Support for People with Oral and Head and Neck Cancer.
CMS consistently denies this type of coverage because of the exorbitant costs associated with often extensive dental treatments, Dr. Sciubba told DrBicuspid.com. Medically related dental treatments can cost more than the surgery and radiation treatment for the underlying medical conditions, he added.
Pending legislation
Some congressmen have introduced laws to help patients like Grass cope with the aftermath of oral cancer treatment.
Support is growing for the U.S. House of Representatives (HR 4091) and the Senate versions (S 1878) of the Coordination of Pro Bono Medically Recommended Dental Care Act. The legislation, which the Academy of General Dentistry supports, would provide grants to organizations that coordinate pro bono, medically necessary dental care.
The bill would help dentists provide care to elderly patients with conditions such as diabetes, cancer, autoimmune disease, and kidney disease and those who need heart or joint replacements. Sen. Robert Menendez (D-NJ), the sponsor of the Senate bill, and Sen. Bernie Sanders (I-VT) are currently working to add similar language to the reauthorization of the Older Americans Act, which could move through the Senate later this year.
Grass, a retired police officer and military veteran, is bitter about the way the government is treating him. “I worked for 25 years as a police officer and served in the U.S. Navy during the Korean War, and this is the kind of treatment I get,” he said.
He was unprepared for the impact of his surgeries. “The doctors don’t tell you what to expect,” Grass said. “Then afterward, all of these problems develop.”
Today, Grass is cancer-free, but he worries that it may return.
“I am supposedly clean of any cancer in my mouth at this point, but whenever I get a toothache or sore mouth, the first thing that enters your mind is that the cancer’s back,” he said. “There’s a monkey on your back for the rest of your life.”
But he remains resolute in his struggle. “If people like me and my wife don’t fight, nothing will be changed.”
This news story was resourced by the Oral Cancer Foundation, and vetted for appropriateness and accuracy.

Leave A Comment
You must be logged in to post a comment.