Recent research conducted at the University of Texas MD Anderson Cancer Center suggests clinical outcomes in patients receiving intensity-modulated radiation therapy (IMRT) for head and neck cancers is more effective when compared to patients who receive traditional radiation therapy, thanks to the advanced technology of IMRT. IMRT precisely targets malignant cells without affecting the normal surrounding tissue, thereby reducing the risk of adverse effects and improving therapy associated effects.
The results of this study were published online in the peer-reviewed journal Cancer.
What is IMRT?
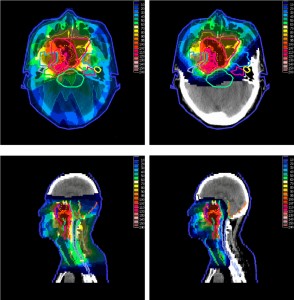
Intensity-modulated radiation therapy, or IMRT, limits the exposure of radiation to normal tissue by employing multiple beams of radiotherapy that helps in setting the dosage by radiologists in accordance with the site and size of tumor.
Assistant professor at MD Anderson’s Radiation Oncology, Beth Beadle explained:
“Previous studies indicated that patients treated with IMRT did better when it came to treatment-related side effects, however these studies were not designed to examine survival. The survival data was not well-known because IMRT is intended to spare normal tissues but still deliver radiation to the tumor so previous models assumed it was equivalent survival at best.”
The technique was approved in 1999, and since then has become increasingly popular mainly because of the high benefits and low toxicity profile. The risk of several common but problematic complications (such as tissue fibrosis, dry mouth, dental issues and musculoskeletal flexibility) can be significantly reduced when compared to conventional radiotherapy.
Details of the research conducted by University of Texas MD Anderson Cancer Center:
The research team used retrospective study design to research the population-based study. The Surveillance, Epidemiology and End Results (SEER) Medicare database was used to choose 3,172 study participants who sought radiotherapy (conventional or IMRT) for head and neck cancer during 1999 – 2007.
Data suggested that IMRT treatment was provided to 1,056 patients and conventional radiotherapy to 2,116. The majority of the head and neck cancers were squamous cell (constituting over 91.2%) but other sub-types were also included. Due to high risk of mortality, the research team set a scoring model to minimize the risk of bias. The scoring system was based on various parameters like age of patients, gender, diagnosis, race, education, income and family history.
Results of the study:
The research team set primary end-point at cause-specific survival (CSS) at 40-months of follow- up. The results reflected a remarkable improvement in the outcome (obtained via scoring system) in patients who received IMRT when compared to those who received conventional radiotherapy. Patients on IMRT scored better on CSS (38.9%) as opposed to those who received conventional therapy (CSS was 18.9%)
Although the research team employed highly sensitive measures, there was still a concern that the results may be biased (considering the possibility of some unmatched variables). To balance this possibility, the team employed instrumental variable model that delivered the same results.
Beadle explained:
“From a scientific perspective, the findings support the use of IMRT and suggests we can provide excellent care while optimizing cancer outcomes and reducing toxicities. At a more global level, with concerns about health care financing and resource allocation, IMRT is more expensive than conventional radiation therapy, but the data suggest it’s worth it.”
The authors also considered another study conducted by Yong that proposed IMRT as a more cost-effective therapy in the setting of oropharynx carcinoma. The study suggested that despite the higher therapy cost, IMRT is superior because of lower risk of toxicity and side-effects (for example lower incremental cost of $4,532 due to lesser risk of xerostomia). Beadle said that additional research is needed to say with precision that IMRT is more cost-effective; nevertheless, lower toxicity definitely improves the overall cost of IMRT over conventional radiotherapy.
Authors also suggested that some limitations always persists in observational studies like negative HPV status of study participants (that may affect the outcome of tumors), uncertain Medicare claims and lack of data on younger patients.
*Photo from Wikipedia.org
** This news story was resourced by the Oral Cancer Foundation, and vetted for appropriateness and accuracy.

Leave A Comment
You must be logged in to post a comment.