Immunotherapy, which aims to harness the body’s immune system to fight off certain cancers, has received plenty of attention, praise and investment in recent years. Breakthrough treatments for melanoma and other cancers have shown startling results, giving some patients months and often years of life they almost certainly would not otherwise have had.
Yet, for all their promise, immune therapies have not produced such dramatic results for the majority of patients. The same drug that causes metastatic melanoma to vanish in one patient might have no effect on another. At best, only one or two patients out of five will respond to immunotherapy treatments — remarkable numbers compared to past standards, but still far lower than anyone would like.
New research published Monday in the journal Nature explores the molecular mechanisms that prevent immunotherapy drugs from working in some patients, and researchers hope the findings will help make the treatments more effective over time.
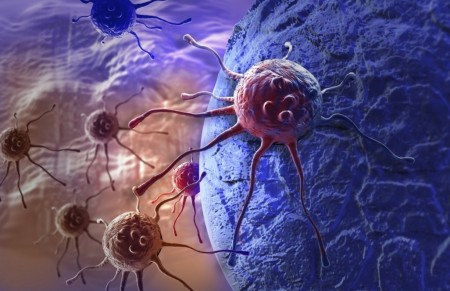
In short, the researchers studied why certain tumors were able to evade immune therapies designed to unleash the body’s defenses to fight cancer. They noted that tumors with a high concentration of “T cells,” a type of white blood cell essential to the human immune system, were more responsive to the treatments. Tumors with a low number of T cells inside what researchers call the “cancer microenvironment” were far less responsive to the new drugs.
“The tumors are acting to protect themselves,” said Weiping Zou, a senior author of the study and a professor of surgery, immunology and biology at the University of Michigan’s medical school. “If the T cells cannot get in, they have no way to kill the tumors.”
Using human and mouse models of ovarian cancer cells, he and other scientists experimented with specific drugs aimed at helping generate more T cells within a tumor, so that it would then be more responsive to immunotherapy. Although it’s early, the approach seems to have promise.
Immune therapies have rapidly become a pillar of cancer treatment in recent years, and numerous trials are underway in hopes of expanding the successes to bladder cancer, breast cancer, Hodgkin’s lymphoma, head and neck tumors, and other types of the disease. Researchers also are testing the new drugs in combination with one another and with other therapies.
The main obstacle has been the realization that some cancers have proved less susceptible to immune therapies, and some patients have fared far better than others. If researchers such as Zou and his colleagues can engineer ways to make game-changing immune therapies effective in more patients, that would be a game-changing feat.
“How can we make the responders more responsive, and make the non-responders become responders?” Zou said. “That’s the whole goal.”

Leave A Comment
You must be logged in to post a comment.